Hey.
I previously shared info on an online workshop, but apparently the link was bad. here’s the revised–and working–link! I hope to see you there!
https://secure.qgiv.com/for/socialworktrainingseries/event/suicideassesment/
Hey.
I previously shared info on an online workshop, but apparently the link was bad. here’s the revised–and working–link! I hope to see you there!
https://secure.qgiv.com/for/socialworktrainingseries/event/suicideassesment/

Tomorrow I’ll be presenting all day on Strengths-Based Suicide Assessment and Treatment at Water’s Edge Counseling Services in Rogers, Arkansas. Water’s Edge Counseling Services employs dozens of therapists at four locations. They continue to grow to meet the mental health needs of Arkansas residents. You can find information about their services here: https://www.watersedgecounselingnwa.com/
In anticipation of tomorrow, I looked up some stats on suicide in Arkansas and the U.S.
Today has been a hard day in Montana, as I’ve heard about two deaths by suicide by individuals in the social world of friends and family. Suicides are tragic and difficult to understand. When suicide happens, it’s important to remember many things, but a couple key points come to mind today.
My big points are that suicide is very difficult to predict and prevent and yet it’s very easy and common for people to feel guilty when someone they know dies of suicide . . . even though the people left behind are not at fault.
However your day has gone today, I wish you as much peace and comfort as possible. If you’re feeling suicidal or especially guilty, please reach out to someone who loves you. They will be happy to talk. Or, if you feel the need, you can call the national suicide crisis hotline: 988. Or, if you’re a texter, there’s a text hotline. Just text HOME to 741741 to connect with a volunteer Crisis Counselor.
All my best to you . . . and here are the ppts for tomorrow’s presentation:
I just finished a nice session on the strengths-based approach to suicide with the NDCA. They asked for a little extra info/emphasis on working with men, because men are particularly vulnerable to suicide, and so I wove in some of the content from my ACA presentation with Matt Englar-Carlson and Dan Salois (thanks Matt and Dan!).
The ppt below is a big one because it includes an embedded video featuring a young man who articulates a number of potential suicide related drivers, including trauma (be forewarned: the content is intense and potentially triggering).
A big thanks to the NDCA organizers and to the attendees who were very impressive.
Have a great evening!

During a couple of my presentations at the ACA conference in Toronto (pictured above) I wasn’t able to fit in some short demonstration videos. To address my time management problems, I’m posting links to them here, along with a short description. Note: All of the videos for suicide demonstrations are non-scripted simulations.
Video 1: An example of an opening of a session with Kennedy, a 15-year-old cisgender white female with a history of suicidal ideation. Key things to watch for include how I immediately mention suicide, focus on sources of distress in Kennedy’s life, and acknowledge things I know and things I don’t know. If we think about emotional distress (aka Shneidman’s psychache) as contributing to suicidality, contemplate what you think is the driver of Kennedy’s feelings of suicidality. The link: https://www.youtube.com/watch?v=gR7YU0VrHqw&t=5s
Video 2: An example of me closing the session with Kennedy using Stanley & Brown’s (2013) Safety Planning Intervention. As always, I’m not perfect in the video, but it shows a process during which I’m trying to cover the safety planning categories in an interpersonally engaging and pleasant manner. The link: https://www.youtube.com/watch?v=jd7PM9HFDO4&t=10s
Video 3: I’m working with Chase, a 35-year-old Gay cisgender male. In this video, I try to get Chase to see a potential pattern of him being suicidal in response to bullying in the past and being interpersonally invalidated in the present. Chase dismisses my “light interpretation” with something like, “That’s the hand I was dealt.” Again, although I’m imperfect in this video, I do take the hint and shift from an abstract interpretation to a concrete assessment process I call the “Social Universe.” During that process, it becomes clear that Chase is spending too much time with “toxic” people in his life and not much time with people who accept him. Additionally, he presents as quite depressed and unable to come up with anyone “validating” and so I shift to a process called, “Building hope from the bottom up” by asking him, “Who’s the least validating or most toxic?” Chase responds pretty well to a process that starts at the bottom or most negative place.” The link: https://www.youtube.com/watch?v=UNBR3bKyE4I&t=7s
Thanks to everyone who attended the ACA conference, for being the kind of professionals who are pursuing awareness, knowledge, and skills in order to be more effective in helping others life meaningful lives. I was humbled by your engagement with the learning process.

Emily Sallee and I had an excellent (and inspiring) day 1 at the 2022 MASP Summer Institute. The MASP members and other participants have been fabulous. Today, we built a foundation upon which we will build great things tomorrow.
What’s up for tomorrow? Advanced treatment planning using the seven-dimensional strengths-based model. Just in case you’re at the Summer Institute OR you want a peek into what we’re doing, here are some handouts.
Last week I had the honor of presenting three times at the American Counseling Association meeting in Atlanta. Today, I’m posting the Abstracts and Powerpoints from those presentations, just in case someone might find the information useful.
On Friday, April 8: The way of the humanist: Illuminating the path from suicide to wellness. Invited presentation on behalf of the Association for Humanistic Counseling.
At this moment, counselors are hearing more distress, anxiety, and suicidal ideation than ever before. In response, we are called to resonate with our clients’ distress. On behalf of the Association for Humanistic Counseling, John Sommers-Flanagan will describe how humanistic principles of acceptance and empathy can paradoxically prepare clients to embrace wellness interventions. Participants will learn five evidence-based happiness strategies to use with their clients and with themselves.
Also, on Friday, April 8: Using a strengths-based approach to suicide assessment and treatment in your counseling practice. Invited presentation on behalf of ACA Publications.
Most counselors agree: no clinical task is more stressful than suicide assessment and treatment planning. When working with people who are suicidal, it’s all-too-easy for counselors to over-focus on psychopathology and experience feelings of hopelessness and helplessness. However, framing suicidal ideation as an unparalleled opportunity to help alleviate your client’s deep psychological pain, and embracing a strengths-based orientation, you can relieve some of your own anxiety. This practice-oriented education session includes an overview of strengths-based principles for suicide assessment and treatment.
On Saturday, April 9, Being seen, being heard: Strategies for working with adolescents in the age of Tik Tok. Educational presentation (with Chinwe Williams).
Counseling and connecting with adolescents can be difficult. In this educational session, we will present six strategies for connecting with and facilitating change among adolescents. For each strategy, the co‐presenters, coming from different cultural and generational perspectives, will engage each other and participants in a discussion of challenges likely to emerge when counseling adolescents. Social media influences, self‐disclosure, and handling adolescents’ questions will be emphasized.
Thanks for reading. I hope some of these resources are helpful to you in your work.
JSF

Apparently, video podcasts are the thing. Or maybe they’ve been a thing for a while. . . or at least since early 2020 and the onset of the Zoom age. I think we should call them vid-pods.
Two weeks ago, I promoted a vid-pod with Paula Fontenelle, Stacey Freedenthal, and me. It was Paula’s vid-pod, titled “Understand Suicide.” Paula is very experienced, very knowledgeable and produces great vid-pods. You can check out all her work, including her podcast (aka vid-pod) at: https://www.understandsuicide.com/
Late last year, Victor Yalom of Psychotherapy.net asked if he could connect me for a possible appearance on a vid-pod called “Normalize the Conversation.” Normalize the Conversation is the brain-child of Francesca Reicherter. Francesca is also the Founder and President of “Inspiring My Generation.” I think Victor wanted me to promote our 7.5-hour marathon Suicide Assessment and Treatment video training series with Psychotherapy.net. . . so here’s the link to that: https://www.psychotherapy.net/videos/expert/john-sommers-flanagan
In contrast to Paula, Stacey, Victor, and me, Francesca is very young. . . and she’s a powerhouse. I’m not sure where she finds the time to do all that she’s doing. She’s 23, but started her mental health advocacy work at age 12. She has published a workbook, founded her own organization, and has over 60 vid-pod episodes online. She’s also a graduate student. You can read more about Francesca here: https://inspiringmygeneration.org/2021/05/28/francesca-reicherter-starting-the-conversation-on-mental-health-conditions/
You can also check out all her vid-pods at: https://podcasts.apple.com/us/podcast/normalize-the-conversation/id1587903841 – The vid-pod with me is from February 2, 2022 and here: https://podcasts.apple.com/us/podcast/what-you-should-know-about-the-clinical-interview/id1587903841?i=1000549745008
Francesca and I did a recording together and she did a bunch of editing and promoting and this past week she sent me some video clips of our time together. What you’ll immediately notice in the video clips is that Francesca is an artist at getting people to talk. Throughout the clips, I’m talking and she’s not. Somehow, she got me to talk for about 47 minutes (although she did some nice summaries and commentary here and there). If my experience is at all representative, I suspect Francesca will be a talented therapist and fabulous listener.
You can check out the vid-pod clips below, but more importantly, check out all the amazing work of Paula, Stacey, Victor, and Francesca . . . all of whom are making the world a place where supportive and quality mental health services are more accessible.
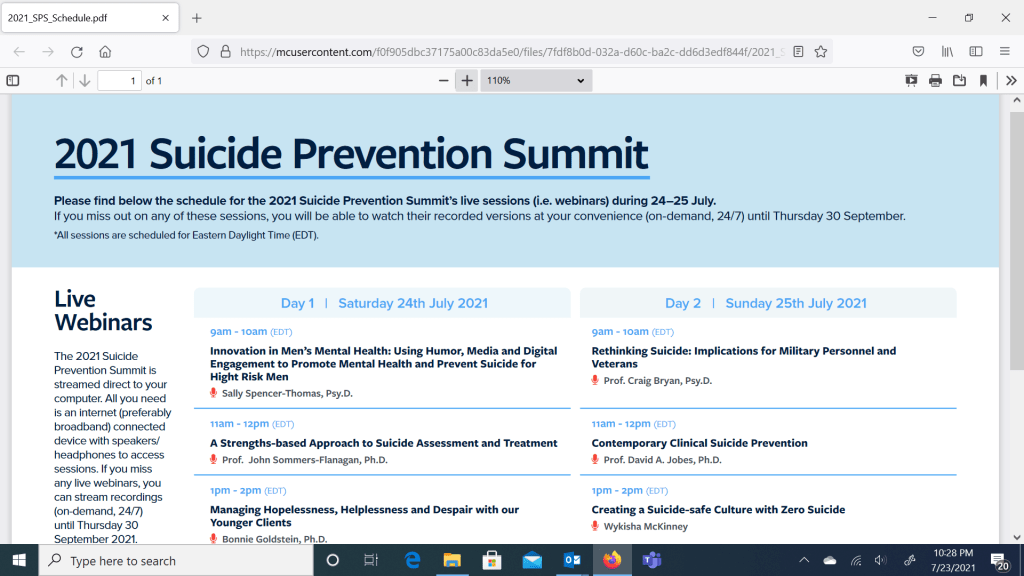
Good morning! The 2021 MHA Suicide Summit has started (see below) and I’ll be up in less than an hour.
Sometimes I think the hardest part about doing workshops is writing the workshop blurb. My problem-and maybe it’s just my problem—is that the process of writing workshop blurbs nearly always impairs my judgment. I start out writing like a sensible and rational person, but eventually I decompensate into displaying delusions of grandeur. For the Mental Health Academy Suicide Summit, I completely lost touch with reality and claimed that I would,
Of course, all of this is great, but, here’s the catch. I’m only presenting for 45 minutes!
If anyone out there can help me become more realistic, I would appreciate the input.
In the meantime, here are the ppts for the presentation today.
John
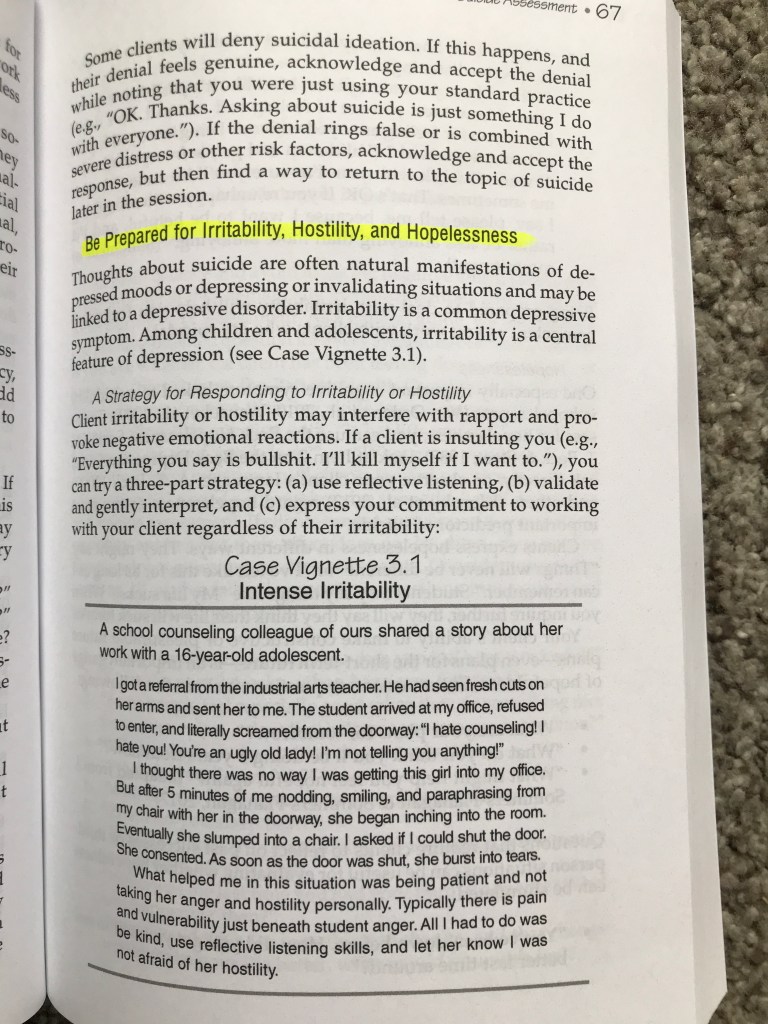
Just for fun, here’s a photo of a page from our Suicide Assessment and Treatment Planning book. This page is the lead in to a section that focuses in on how to work with clients who are suicidal, but whom also may be naturally also experiencing irritability, hostility, and hopelessness. For info, go to the publisher, ACA: https://imis.counseling.org/store/detail.aspx?id=78174

The following is another excerpt from a chapter I wrote with my colleagues Roni Johnson and Maegan Rides At The Door. This excerpt focuses on ways in which clinical interviews are used as assessment tools. The full chapter is forthcoming in the Cambridge Handbook of Clinical Assessment and Diagnosis. For more (much more) information on clinical interviewing, see our textbook, creatively titled, Clinical Interviewing, now in its 6th edition. If you’re a professor or college instructor, you can get a free evaluation copy here: https://www.wiley.com/en-us/Clinical+Interviewing%2C+6th+Edition-p-9781119215585
The clinical interview often involves more assessment and less intervention. Interviewing assessment protocols or procedures may not be limited to initial interviews; they can be woven into longer term assessment or therapy encounters. Allen Frances (2013), chair of the DSM-IV task force, recommended that clinicians “be patient,” because accurate psychiatric diagnosis may take “five minutes. . .” “five hours. . .” “five months, or even five years” (p. 10).
Four common assessment interviewing procedures are discussed next: (1) the intake interview, (2) the psychodiagnostic interview, (4) mental status examinations, and (4) suicide assessment interviewing.
The Intake Interview
The intake interview is perhaps the most ubiquitous clinical interview; it may be referred to as the initial interview, the first interview, or the psychiatric interview. What follows is an atheoretical intake interview model, along with examples of how theoretical models emphasize or ignore specific interview content.
Broadly speaking, intake interviews focus on three assessment areas: (1) presenting problem, (2) psychosocial history, and (3) current situation and functioning. The manner in which clinicians pursue these goals varies greatly. Exploring the client’s presenting problem could involve a structured diagnostic interview, generation and analysis of a problem list, or clients free associating to their presenting problem. Similarly, the psychosocial history can be a cursory glimpse at past relationships and medical history or a rich and extended examination of the client’s childhood. Gathering information about the client’s current situation and functioning can range from an informal query about the client’s typical day to a formal mental status examination (Yalom, 2002).
Psychodiagnostic Interviewing
The psychodiagnostic interview is a variant of the intake interview. For mental health professionals who embrace the medical model, initial interviews are often diagnostic interviews. The purpose of a psychodiagnostic interview is to establish a psychiatric diagnosis. In turn, the purpose of psychiatric diagnosis is to describe the client’s current condition, prognosis, and guide treatment.
Psychodiagnostic interviewing is controversial. Some clinicians view it as essential to treatment planning and positive treatment outcomes (Frances, 2013). Others view it in ways similar to Carl Rogers (1957), who famously wrote, “I am forced to the conclusion that … diagnostic knowledge is not essential to psychotherapy. It may even be … a colossal waste of time” (pp. 102–103). As with many polarized issues, it can be useful to take a moderate position, recognizing the potential benefits and liabilities of diagnostic interviewing. Benefits include standardization, a clear diagnostic focus, and identification of psychiatric conditions to facilitate clinical research and treatment (Lilienfeld, Smith, & Watts, 2013). Liabilities include extensive training required, substantial time for administration, excess structure and rigidity that restrain experienced clinicians, and questionable reliability and validity, especially in real-world clinical settings (Sommers-Flanagan & Sommers-Flanagan, 2017).
Clinicians who are pursuing diagnostic information may integrate structured or semi-structured diagnostic interviews into an intake process. The research literature is replete with structured and semi-structured diagnostic interviews. Clinicians can choose from broad and comprehensive protocols (e.g., the Structured Clinical Interview for DSM-5 Disorders – Clinician Version; First et al., 2016) to questionnaires focusing on a single diagnosis (e.g., Autism Diagnostic Interview – Revised; Zander et al., 2017). Additionally, some diagnostic interviewing protocols are designed for research purposes, while others help clinicians attain greater diagnostic reliability and validity. Later in this chapter we focus on psychodiagnostic interviewing reliability and validity.
The Mental Status Examination
The MSE is a semi-structured interview protocol. MSEs are used to organize, assess, and communicate information about clients’ current mental state (Sommers-Flanagan, 2016; Strub & Black, 1977). To achieve this goal, some clinicians administer a highly structured Mini-Mental State Evaluation (MMSE; Folstein, Folstein, & McHugh, 1975), while others conduct a relatively unstructured assessment interview but then organize their observations into a short mental status report. There are also clinicians who, perhaps in the spirit of Piaget’s semi-clinical interviews, combine the best of both worlds by integrating a few structured MSE questions into a less structured interview process (Sommers-Flanagan & Sommers-Flanagan, 2017).
Although the MSE involves collecting data on diagnostic symptoms, it is not a psychodiagnostic interview. Instead, clinicians collect symptom-related data to communicate information to colleagues about client mental status. Sometimes MSEs are conducted daily or hourly. MSEs are commonly used within medical settings. Knowledge of diagnostic terminology and symptoms is a prerequisite to conducting and reporting on mental status.
Introducing the MSE. When administering an MSE, an explanation or role induction is needed. A clinician might state, “In a few minutes, I’ll start a more formal method of getting … to know you. This process involves me asking you a variety of interesting questions so that I can understand a little more about how your brain works” (Sommers-Flanagan & Sommers-Flanagan, 2017, pp. 580–581).
Common MSE domains. Depending on setting and clinician factors, the MSE may focus on neurological responses or psychiatric symptoms. Nine common domains included in a psychiatric-symptom oriented MSE are
Given that all assessment processes include error and bias, mental status examiners should base their reports on direct observations and minimize interpretive statements. Special care to cross-check conclusive statements is necessary, especially when writing about clients who are members of traditionally oppressed minority groups (Sommers-Flanagan & Sommers-Flanagan, 2017). Additionally, using multiple assessment data sources (aka triangulation; see Using multiple (collateral) data sources) is essential in situations where patients may have memory problems (e.g., confabulation) or be motivated to over- or underreport symptoms (Suhr, 2015).
MSE reports. MSE reports are typically limited to one paragraph or one page. The content of an MSE report focuses specifically on the previously listed nine domains. Each domain is addressed directly with at least one statement.
Suicide Assessment Interviewing
The clinical interview is the gold standard for suicide assessment and intervention (Sommers-Flanagan, 2018). This statement is true, despite the fact that suicide assessment interviewing is not a particularly reliable or valid method for predicting death by suicide (Large & Ryan, 2014). The problem is that, although standardized written assessments exist, they are not a stand-alone means for predicting or intervening with clients who present with suicide ideation. In every case, when clients endorse suicide ideation on a standardized questionnaire or scale, a clinical interview follow-up is essential. Although other assessment approaches exist, they are only supplementary to the clinical interview. Key principles for conducting suicide assessment interviews are summarized below.
Contemporary suicide assessment principles. Historically, suicide assessment interviewing involved a mental health professional conducting a systematic suicide risk assessment. Over the past two decades, this process has changed considerably. Now, rather than taking an authoritative stance, mental health professionals seek to establish an empathic and collaborative relationship with clients who are suicidal (Jobes, 2016). Also, rather than assuming that suicide ideation indicates psychopathology or suicide risk, clinicians frame suicide ideation as a communication of client distress. Finally, instead of focusing on risk factors and suicide prediction, mental health professionals gather information pertaining to eight superordinate suicide dimensions or drivers and then work with suicidal clients to address these dimensions through a collaborative and therapeutic safety planning process (Jobes, 2016). The eight superordinate suicide dimensions include:
(For additional information on suicide assessment interviewing and the eight suicide dimensions, see other posts on this site).