Why Do We Need a Strengths-Based Approach to Suicide Assessment and Treatment?
Imagine this: You’re living in a world that seems like it would just as soon forget you exist. Maybe your skin color is different than the dominant people who hold power. Maybe you have a disability. Whatever the case, the message you hear from the culture is that you’re not important and not worthy. You feel oppressed, marginalized, unsupported, and as if much of society would just as soon have you become invisible or go away.
In response, you intermittently feel depressed and suicidal. Then, when you enter the office of a health or mental health professional, the professional asks you about depression and suicide. Even if the professional is well-intended, judgment leaks through. If you admit to feeling depressed and having suicidal thoughts, you’ll get a diagnosis that implies you’re to blame for having depressing and suicidal thoughts.
The medical model overfocuses on trying to determine: “Are you suicidal?” The medical model is also based on the assumption that the presence of suicidality indicates there’s something seriously wrong with you. But if we’re working with someone who has been or is currently being marginalized, a rational response from the patient might be:
“As it turns out, I’ve internalized systemic and intergenerational racism, sexism, ableism, and other dehumanizing messages from society. I’ve been devalued for so long and so often that now, I’ve internalized societal messages: I devalue myself and wonder if life is worth living. And now, you’re blaming me with a label that implies I’m the problem!”
No wonder most people who are feeling suicidal don’t bother telling their health professionals.
When I think of this preceding scenario, I want to add profanity into my response, so I can adequately convey that it’s completely unjust to BLAME patients for absorbing repeated negative messages about people who look like or sound like or act like them. WTH else do you think should happen?
This is why we need to integrate strengths-based principles into traditional suicide assessment and prevention models. Of course, we shouldn’t use strengths-based ideas in ways that are toxically positive. We ALWAYS need to start by coming alongside and feeling with our patients and clients. As it turns out, if we do a good job of coming alongside patients/clients who are in emotional pain, natural opportunities for focus on strengths and resources, including cultural, racial, sexual, and other identities that give the person meaning.
I’m reminded of an interview I did with an Alaskan Native person from the Yupik tribe. She talked at length about her depression, about feeling like a zombie, and past and current suicidal thoughts. Eventually, I inquired: “What’s happening when you’re not having thoughts about suicide?” She seemed surprised. Then she said, “I’d be singing or writing poetry.” I instantly had a sense that expressing herself held meaning for her. In particular, her singing Native songs and contemporary pop songs became important in our collaborative efforts to build her a safety plan.
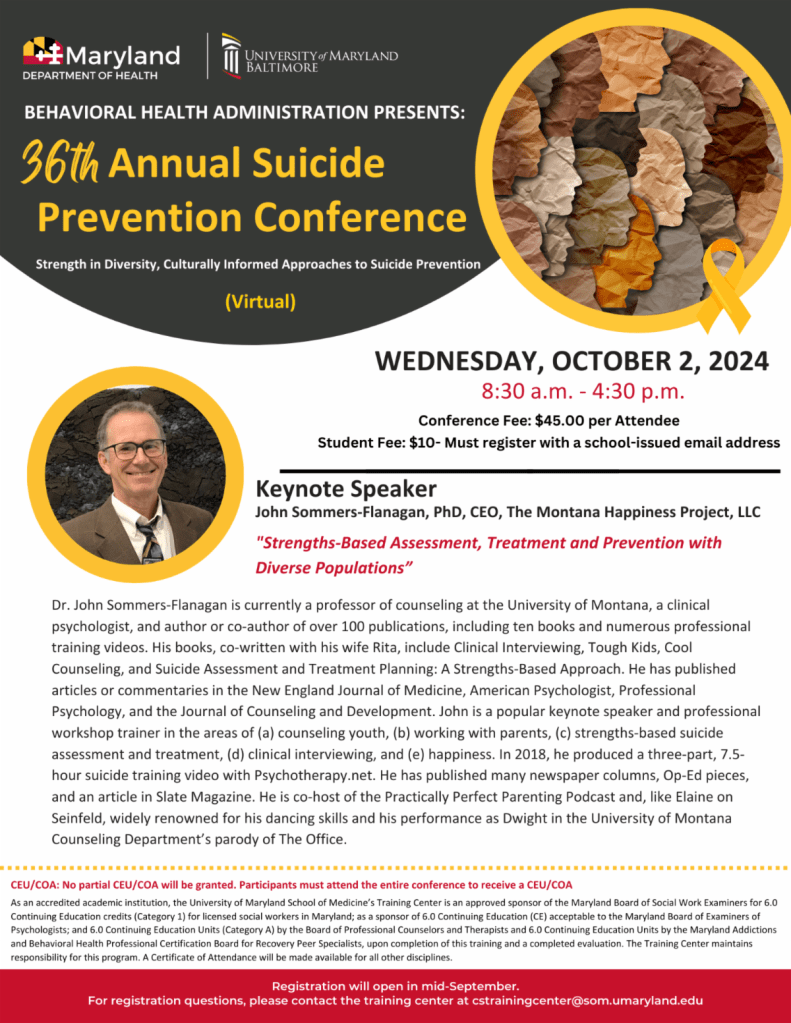
This coming Wednesday morning I have the honor of presenting as the keynote speaker for the Maryland Department of Health 36th Annual Suicide Prevention Conference. During this keynote, I’ll share more ideas about why a strengths-based model is a good fit when working with diverse clients who are experiencing suicidal thoughts and impulses.
With all that said, here’s the title and abstract of my upcoming presentation.
Strengths-Based Assessment, Treatment, and Prevention with Diverse Populations
Traditional suicide assessment tends to be a top-down information-gathering process wherein healthcare or prevention professionals use questionnaires and clinical interviews to determine patient or client suicide risk. This approach may not be the best fit for people from populations with historical trauma, or for people who continue to experience oppression or marginalization. In this presentation, John Sommers-Flanagan will review principles of a strengths-based approach to suicide prevention, assessment, and treatment. He will also discuss how to be more sensitive, empowering, collaborative, and how to leverage cultural strengths when working with people who are potentially suicidal. You will learn at least three practical strengths-based strategies for initiating conversations about suicide, conducting culturally-sensitive assessments, and implementing suicide interventions—that you can immediately use in your prevention work.
